Four Stages of Osteoarthritis
The four stages of osteoarthritis extend over several years, even decades. Often the disease is not detected until it reaches an advanced stage. This is usually when there are the first signs of movement restrictions or pain.
Since the disease is well developed by this time, there is little that can be done to reverse the condition. The most common conventional approach to treatment is participation in specific exercise regimes and reliance on pain killers. Eventually, the affect joint(s) may require replacement with a metal implant.
The severity of arthritic disease is assessed according to four stages of osteoarthritis. Here, the fibre damage in articular cartilage plays an equally important role as the degree of involvement of the underlying bone.
Stage 1: Shows only a slight fraying of the articular cartilage mostly due to falls, blows or other injuries. This is caused by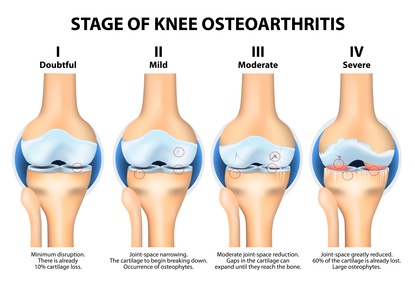 slightly roughened articular cartilage surfaces rubbing against each. Particles can detach that reinforce this friction.
slightly roughened articular cartilage surfaces rubbing against each. Particles can detach that reinforce this friction.
Stage 2: Characterised by significant fibre damage in articular cartilage. The surface is rough and covered with indentations and raised portions. This has a further negative impact on joint structure.
Stage 3: This is the transition stage and where deep cartilage destruction starts. It’s often associated with pain and restricted mobility. Joint inflammation is common.
Stage 4: This is the final stage of the disease with a complete loss of joint cartilage. This is associated with more serious deformation and disruption of the underlying bone. The pain is typically severe and pain relief ineffective. Movement is so restricted that the only option is a prosthetic replacement of the joint.
Symptoms of Arthrosis
Each of the above-mentioned four stages of osteoarthritis is characterised by a range of symptoms. As the disease progresses, the symptoms also become more prevalent. The problem with osteoarthritis is that the initial defect is very common in childhood or early adolescence. A bruised knee or a twisted wrist heals quickly again and all is forgotten.
However, these minor injuries can directly impact the cartilage or affect the nutrient supply to the cartilage. This can result in increased friction of the joint surfaces. Over time, this friction continues to damage the joint and osteoarthritis develops. Recognising the onset of osteoarthritis early on is the key to effective treatment.
The symptoms are initially very diverse and specific. Usually it starts with pain in the affected joint after periods of immobility. This is most obvious in the morning or after prolonged sitting. The joints feel stiff and take a few minutes to loosen up. As the joints start to move more freely, the joint surfaces become lubricated by the synovial fluid. This lubrication reduces the friction and the joints don’t feel stiff anymore.
As the disease progresses, pain increases as the joints become further stresses. Walking long distances can lead to aches in the affected knee or hip joints. After a break, it’s possible to continue to move relatively pain-free again. That is until a certain distance has been covered and then the cycle is repeated.
With the progressive destruction of the cartilage the pain becomes more permanently. Joint mobility is also reduced to the point of stiffness. Now the previously relatively “silent” disease transforms into an activated form of arthrosis. Ligaments and tendons next to the joints also become inflamed. This can lead to scaring and further exacerbate athrosis symptoms.
The sooner symptoms of arthrosis are identified; the easier it is to protect the joint. Taking measures early on to protect cartilage is essential for preventing or slowing down the onset of osteoarthritis. This may be enough to avoid joint surgery and joint replacements.





